The cost of ACA (Affordable Care Act) Marketplace plans in 2025 varies significantly based on your age, location, household size, and income level—especially due to eligibility for subsidies and cost-sharing reductions. Here's a breakdown:
💵 Average Monthly Premiums (2026)
- Silver plans for a 40-year-old average approximately $621/month before subsidies.
- Bronze plans average around $380–$495/month.
- Gold plans average about $510–$676/month.
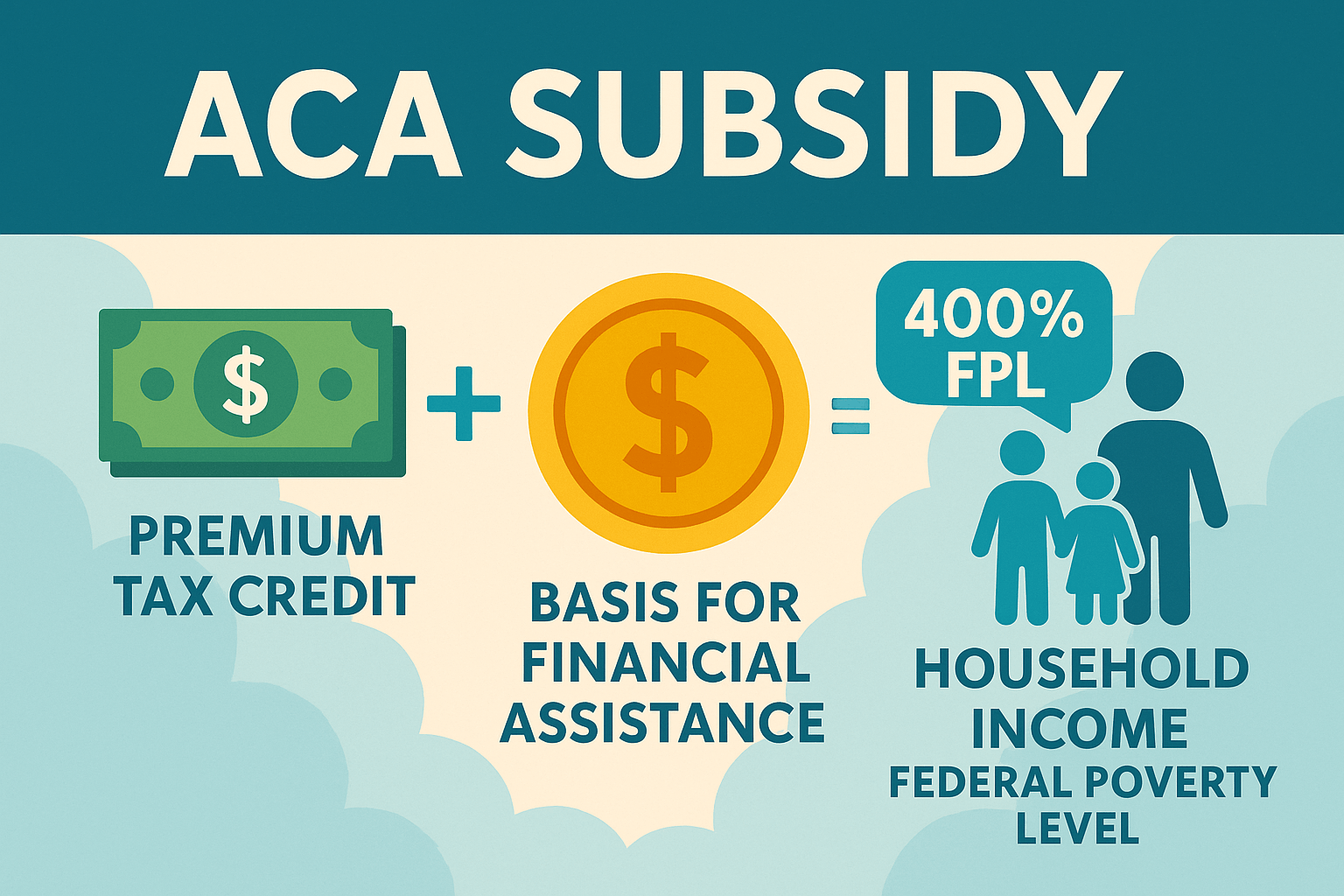
Most enrollees qualify for premium tax credits, reducing actual costs—over 4 in 5 pay just $10/month or less
🏛️ Premium Assistance & Key Savings
- The Premium Tax Credit (PTC) limits what you pay for the benchmark Silver plan to between 0% and 8.5% of household income, depending on your income relative to the Federal Poverty Level (FPL).
- Cost-Sharing Reductions (CSRs) are available for individuals with incomes up to about 250% of FPL, often leading to deductibles as low as $90 when enrolled in a CSR-eligible Silver plan.
📊 Out-of-Pocket Maximum:
The most you’ll pay in a year before your plan covers 100% of costs. ACA caps this (e.g., ~$10,600 for individuals and ~$21,000 for families in 2026).
💳 Annual Deductibles:
The amount you pay out-of-pocket before your insurance begins paying.
🩺 Average Annual Deductibles (2026):
- Silver plan deductibles are around $5,304 more.
- Bronze plan deductibles may reach up to $9,000.
Copayments and Coinsurance:
Shared costs for specific services or prescriptions after your deductible is met.